Weight is often discussed in terms of appearance, confidence, or clothing size. However, from a medical and public health perspective, excess body weight—particularly belly fat—is closely linked to a wide range of chronic health conditions that affect almost every system in the body (World Health Organization, 2024).
These health problems are known as weight-related conditions, weight-related conditions affect multiple organs in the body and are strongly linked to excess body fat and poor metabolic health.
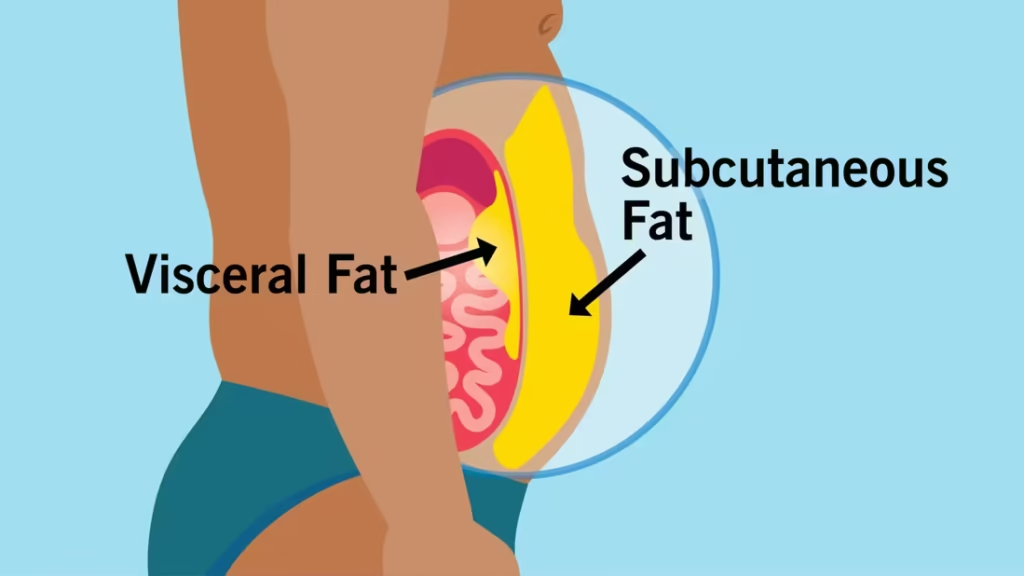
Weight-related conditions refer to health problems that develop or worsen due to excess body fat, especially fat stored around the abdomen. This type of fat, often called visceral fat, is more harmful than fat stored under the skin because it interferes with normal metabolic processes in the body.
In the UK, it is estimated that around 1 in every 4 adults and about 1 in every 5 children aged 10 to 11 are living with obesity (NHS, 2025). Across African communities—both on the continent and in the diaspora—rates of obesity, type 2 diabetes, high blood pressure, and fatty liver disease are rising rapidly (WHO, 2025). Many people are living with these conditions without realising that they are connected, and that excess weight is often the common underlying factor (NHS, 2023).
This pillar guide explains what weight-related conditions are, how they develop, and why managing weight is ultimately about protecting health and preventing disease, not chasing a number on the scale.
Table of Contents
ToggleWhat Are Weight-Related Conditions?
Weight-related conditions are health problems that are caused by or worsened by excess body fat, especially visceral (abdominal) fat (Johns Hopkins Medicine, 2023).
When excess fat accumulates in the body, it:
Disrupts hormone balance
Increases inflammation
Worsens insulin resistance
Places stress on organs such as the liver, heart, and joints
According to the World Health Organization, overweight and obesity significantly increase the risk of non-communicable diseases, including cardiovascular disease, diabetes, and musculoskeletal disorders (WHO, 2024).
Importantly, a person does not need to be “very fat” to develop weight-related conditions. Where fat is stored matters more than body size alone (Després, 2012).
Why Belly Fat Is More Dangerous Than Other Fat
Belly fat, also known as visceral fat, is stored deep inside the abdomen around vital organs such as the liver and pancreas. Unlike fat under the skin, visceral fat is metabolically active (Després, 2012).
It releases inflammatory substances and hormones that:
Worsen insulin resistance
Raise blood pressure
Increase fat storage in the liver
Increase the risk of heart disease
This is why waist circumference is often a stronger predictor of health risk than body weight or BMI alone (NICE, 2025).

How Excess Weight Affects Metabolic Health
Excess weight affects the body mainly through insulin resistance.
When cells stop responding properly to insulin:
Blood sugar levels rise
Insulin levels stay chronically high
Fat storage increases
Inflammation worsens
This creates the foundation for many weight-related conditions to develop together—a pattern commonly referred to as metabolic syndrome (Alberti et al., 2009; Swarup, 2024).
👉 Read more related posts:
Metabolic Syndrome Explained: How High Blood Pressure, Diabetes, and Fatty Liver Are All Connected
9 Weight-Related Conditions You Should Know About
1. Type 2 Diabetes
Excess weight, especially around the abdomen, is one of the strongest risk factors for type 2 diabetes. Insulin resistance develops gradually, often years before diagnosis (Shin et al., 2013).
How excess weight contributes
Excess body fat, particularly visceral fat, interferes with how insulin works in the body. Over time, the pancreas is forced to produce more insulin to keep blood sugar levels stable. Eventually, this system becomes overwhelmed, leading to persistently high blood sugar levels and the development of type 2 diabetes.
Why this matters
Many people live with insulin resistance for years without symptoms. By the time diabetes is diagnosed, damage to blood vessels, nerves, and organs may already be occurring. Early weight management can significantly delay or prevent progression.
👉 Related post: Early Signs of High Blood Pressure You Shouldn’t Ignore
2. High Blood Pressure (Hypertension)
Extra body fat increases blood volume, inflammation, and strain on blood vessels, leading to persistently high blood pressure (Hall et al., 2015; NHS, 2023).
How weight affects blood pressure
Excess weight forces the heart to work harder to pump blood throughout the body. Fat tissue also releases substances that stiffen blood vessels and interfere with normal kidney function, leading to salt and fluid retention.
Why it is often overlooked
High blood pressure often has no obvious symptoms. Many people feel “fine” while silent damage is occurring to the heart, brain, kidneys, and eyes. Weight reduction can lead to measurable improvements in blood pressure control.
👉 Related post: Early Signs of High Blood Pressure You Shouldn’t Ignore
3. Fatty Liver Disease
When excess fat accumulates in the liver, it leads to fatty liver disease, now increasingly referred to as metabolic dysfunction-associated steatotic liver disease (MASLD). Many people have no symptoms until liver damage progresses (Younossi et al., 2023).
How weight affects the liver
Excess calories—especially from sugar and refined carbohydrates—are converted into fat by the liver. Over time, this fat builds up within liver cells, impairing liver function.
Why early detection is important
Fatty liver disease can progress to liver inflammation, fibrosis, and even cirrhosis if left untreated. The encouraging news is that early-stage fatty liver disease is often reversible with lifestyle changes.
4. Heart Disease
Weight-related conditions increase cholesterol abnormalities, inflammation, and blood vessel damage, significantly raising the risk of heart attack and stroke (Mottillo et al., 2010).
The chain reaction
Excess weight often leads to high LDL cholesterol, low HDL cholesterol, high triglycerides, and chronic inflammation. Together, these factors accelerate plaque buildup in arteries.
Long-term impact
Heart disease remains one of the leading causes of death worldwide. Managing weight-related risk factors early plays a crucial role in preventing cardiovascular events later in life.
👉 Related post: Early Signs of Fatty Liver Disease You Shouldn’t Ignore
5. Joint and Knee Problems
Excess weight places mechanical stress on joints, particularly the knees and hips, increasing the risk of osteoarthritis and chronic pain (Arthritis Research UK, 2022).
The mechanical burden
Every extra kilogram of body weight adds several kilograms of pressure across weight-bearing joints. Over time, this accelerates cartilage breakdown.
Quality of life implications
Joint pain can limit mobility, making physical activity more difficult and creating a cycle where reduced movement leads to further weight gain.
6. Sleep Apnoea
Fat deposits around the neck and upper airway can obstruct breathing during sleep, leading to sleep apnoea, poor sleep quality, and daytime fatigue (NHS, 2023).
Why sleep apnoea is dangerous
Repeated interruptions in breathing reduce oxygen levels and strain the heart. Sleep apnoea is strongly linked to high blood pressure, heart disease, and insulin resistance.
Signs to watch for
Loud snoring, morning headaches, excessive daytime sleepiness, and poor concentration may indicate an underlying sleep disorder related to excess weight.
7. Hormonal Imbalance and Fertility Issues
Excess weight can disrupt hormones, contributing to conditions such as polycystic ovary syndrome (PCOS), irregular periods, and reduced fertility in women, as well as low testosterone in men (Teede et al., 2018).
How fat tissue affects hormones
Fat tissue is hormonally active and can interfere with normal reproductive hormone regulation. This can disrupt ovulation in women and reduce testosterone levels in men.
Reproductive and emotional impact
Hormonal imbalance can affect fertility, mood, energy levels, and overall wellbeing. Weight management often improves hormonal balance and reproductive outcomes.
8. Stroke Risk
High blood pressure, diabetes, and abnormal cholesterol—often linked to excess weight—significantly increase stroke risk (WHO, 2024).
Why weight matters
Excess weight contributes to blood vessel damage, clot formation, and irregular heart rhythms, all of which raise stroke risk.
Prevention focus
Managing blood pressure, blood sugar, and weight together provides the strongest protection against stroke.
9. Certain Cancers
Obesity is associated with an increased risk of several cancers, including breast, colorectal, and endometrial cancer, due to chronic inflammation and hormonal changes (World Cancer Research Fund, 2023).
The inflammation link
Chronic low-grade inflammation and elevated insulin levels create an environment that can promote abnormal cell growth.
Long-term risk reduction
Maintaining a healthy weight, staying active, and improving diet quality are important strategies for reducing cancer risk over the lifespan.
👉 Related post: Type 2 Diabetes Explained
Why Weight-Related Conditions Are Rising in Africans
Several factors contribute to the rise of weight-related conditions in African populations:
Increased consumption of ultra-processed foods
Sugary drinks and refined carbohydrates
Sedentary lifestyles
Chronic stress
Late diagnosis and limited routine screening
The World Health Organization reports that non-communicable diseases now account for a growing proportion of deaths in Africa (WHO, 2024).
Can Weight-Related Conditions Be Prevented or Reversed?
Yes—especially when addressed early.
Clinical evidence shows that losing just 5–10% of body weight can improve blood sugar control, lower blood pressure, reduce liver fat, and improve cholesterol levels (NICE, 2015; ADA, 2024).

Practical Steps to Reduce Health Risks (Not Just Lose Weight)
Lifestyle interventions including improved diet quality, reduced sugar intake, regular physical activity, adequate sleep, and stress management have been shown to improve metabolic health and reduce visceral fat (WHO, 2024; NICE, 2025).
Weight Loss vs Metabolic Health: An Important Difference
Not everyone with excess weight is unhealthy, and not everyone with a “normal” weight is metabolically healthy.
The true goal is metabolic health, not just weight reduction (Després, 2012).
Conclusion
Weight-related conditions are not simply about body size or appearance—they are about long-term health, quality of life, and disease prevention. Excess weight, particularly around the abdomen, places ongoing stress on the body and increases the risk of multiple conditions developing at the same time.
The good news is that many weight-related conditions can be prevented, improved, or even reversed when addressed early. Small, consistent lifestyle changes—such as improving diet quality, increasing daily movement, prioritising sleep, and managing stress—can lead to meaningful improvements in metabolic health.
Addressing weight-related conditions early can significantly reduce long-term health risks and improve overall wellbeing.
Rather than focusing solely on weight loss, the goal should be better metabolic health: healthier blood sugar levels, improved blood pressure, reduced liver fat, and lower inflammation. These changes not only reduce disease risk but also support energy levels, mobility, and overall wellbeing.
Understanding weight-related conditions is the first step. Taking informed, sustainable action is the next. With the right knowledge and support, protecting your health is achievable—one step at a time.
References (Harvard Style)
Alberti, K.G.M.M. et al. (2009) ‘Harmonizing the metabolic syndrome’, Circulation, 120(16), pp. 1640–1645.
American Diabetes Association (2024) Standards of Care in Diabetes.
Després, J-P. (2012) ‘Body fat distribution and risk of cardiovascular disease’, Circulation, 126(10), pp. 1301–1313.
Hall, J.E. et al. (2015) ‘Obesity-induced hypertension’, Circulation Research, 116(6), pp. 991–1006.
Johns Hopkins Medicine (2023) Metabolic Syndrome.
Mottillo, S. et al. (2010) ‘The metabolic syndrome and cardiovascular risk’, Journal of the American College of Cardiology, 56(14), pp. 1113–1132.
National Health Service (NHS) (2023) Obesity and related conditions.
NICE (2015) Type 2 diabetes in adults: management (NG28).
NICE (2025) Overweight and obesity management (NG246).
Shin, J.A. et al. (2013) ‘Metabolic syndrome as a predictor of type 2 diabetes’, Diabetes Care, 36(2), pp. 428–435.
Swarup, S. (2024) Metabolic Syndrome, StatPearls.
World Cancer Research Fund (2023) Body fatness and cancer risk.
World Health Organization (2024) Obesity and noncommunicable diseases.
Pingback: New Food Pyramid Explained: Why “Eat Real Food” Matters
Pingback: Kidney and Liver Problems in Nigerian Children: Causes, Symptoms & Prevention
Pingback: 7 Early Signs of Kidney Disease You Should Not Ignore (Diabetes & High Blood Pressure Risk)